
CBG/CBD Oil for Chemotherapy‑Induced Peripheral Neuropathy
July 9, 2025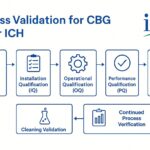
Process Validation and Stability Testing of Cannabigerol
August 27, 2025Cannabigerol Benefits and Research
Cannabigerol is attracting significant interest due to its unique pharmacological profile and therapeutic potential. Notably, CBG interacts only weakly with canonical cannabinoid receptors (CB₁ and CB₂) – it is a partial agonist at these receptors with relatively low affinity. In contrast, CBG shows high potency at non-cannabinoid targets: it is a nanomolar agonist at α2-adrenergic receptors and an antagonist at 5-HT1A serotonin receptors. CBG can also block certain ion channels (e.g. TRPM8) and influence other signaling pathways. These molecular actions differentiate CBG from better-known cannabinoids like CBD and THC, and help explain some of the distinctive effects observed in preclinical studies – for example, anxiolytic (anti-anxiety) effects without intoxication, and potential neuroprotective benefits. At the same time, potent α2-agonism means CBG can suppress noradrenergic activity, which raises safety considerations (sedation, bradycardia, hypotension) that will be discussed later. In summary, CBG’s receptor pharmacology suggests it may “calm” the nervous system via 5-HT1A and α2 pathways, protect neurons, and even enhance certain functions, but also demands careful physiological monitoring.
Cannabigerol and the Nervous System: Anxiolytic and Neuroprotective Potential
Early evidence points to central nervous system (CNS) activity of CBG despite its weak direct action on CB₁/CB₂. In animal models, CBG has demonstrated anxiolytic and antidepressant-like effects. For example, rodent stress paradigms show that CBG treatment can reduce depressive-like immobility (in the mouse tail-suspension test) without producing cannabis-like behavioral impairment. Such preclinical findings align with CBG’s receptor profile – agonism at α2-adrenergic receptors (similar to sedative anxiolytics like clonidine) and antagonism of 5-HT1A (which can modulate anxiety circuits) likely mediate these effects. CBG has also shown neuroprotective properties in models of neurodegenerative disease. In a 2015 study of Huntington’s disease models, CBG was extraordinarily active as a neuroprotectant: it preserved striatal neurons and motor function in toxin-lesioned mice, reduced inflammatory microglial activation, and even partially normalized expression of disease-related genes in a genetic HD mouse strain. The CBG-treated mice had less neuroinflammation and neuronal loss than controls, suggesting CBG can protect neurons under toxic or mutant protein stress. Such findings have spurred interest in CBG for other neurological conditions (e.g. Parkinson’s, multiple sclerosis), especially given its multi-target anti-inflammatory profile.
Human Data on Anxiety and Stress
Until recently, clinical data on CBG in humans were virtually nonexistent. This is rapidly changing. In mid-2024, researchers published the first controlled trial of CBG in healthy human volunteers – a double-blind, placebo-controlled crossover study evaluating acute effects on anxiety, stress, and mood. In this trial (n=34), a single 20 mg oral dose of CBG produced a significant reduction in self-reported anxiety and stress relative to placebo. The magnitude of effect was notable: on average, participants’ anxiety/stress ratings dropped by roughly 20–30% shortly after CBG dosing, whereas no improvement occurred with placebo. Subjects also showed an unexpected enhancement in memory performance, recalling more words on a verbal memory test after CBG than after placebo. Crucially, no cognitive or motor impairments were observed – CBG did not cause the intoxication, euphoria, or performance deficits associated with THC. Participants reported only minimal side effects (no significant changes in dry mouth, appetite, etc.), and rated the experience as essentially non-intoxicating. These findings confirm that CBG can acutely “calm” the nervous system – reducing subjective anxiety/stress – without the trade-off of sedation or mental clouding. They also suggest CBG may even “enhance” certain CNS functions (in this case, memory) in the short term. While intriguing, the investigators caution that these results are preliminary and specific to a single low dose in healthy cannabis-experienced adults. Larger trials in patients with anxiety disorders (and trials examining repeated dosing) are needed to establish efficacy and safety before any therapeutic claims can be made. Nonetheless, the human proof-of-concept data align with the preclinical profile: CBG engages CNS pathways to reduce anxiety, apparently via non-cannabinoid receptor mechanisms, and does so with good tolerability.
Beyond anxiety, researchers are beginning to explore CBG in other CNS contexts. Surveys of CBG users (by self-report) have noted high interest in CBG for pain, mood, and sleep issues. There is also preclinical evidence that CBG could benefit neuroinflammatory and neurodegenerative conditions. As mentioned, CBG improved outcomes in Huntington’s disease mouse models. Additional cell and animal studies suggest anti-inflammatory and antioxidant effects in the CNS, which could translate to neuroprotection in diseases like Parkinson’s or MS. These possibilities remain speculative but biologically plausible – for instance, CBG’s activation of α2-adrenergic receptors might confer some neuroprotective benefit by reducing excessive glutamate release and excitotoxicity, as has been observed with other α2-agonists in brain injury models. Overall, the CNS profile of CBG – anxiolytic, possibly antidepressant and neuroprotective, without impairment – is encouraging, and warrants deeper investigation in clinical contexts such as generalized anxiety, PTSD, and early-stage neurodegenerative diseases. Researchers are already planning Phase-II trials in some of these areas (e.g. CBG for anxiety disorders in the 20–40 mg dose range, as well as combination trials for pain) in order to build on the positive signals seen so far.
Gastrointestinal Effects of Cannabigerol: Inflammation, Gut Barrier, and Microbiome
One of the most promising avenues for CBG is in gastrointestinal (GI) disorders – specifically, inflammatory bowel diseases and related conditions involving gut inflammation and epithelial barrier dysfunction. Unlike THC (which can modulate gut motility via CB₁) or CBD (with broad anti-inflammatory effects), CBG appears to target GI inflammation through a unique mix of cannabinoid and non-cannabinoid pathways. Preclinical studies have demonstrated that CBG can ameliorate colitis, restore intestinal barrier integrity, and even favorably shift the gut microbiome:
- Colon Inflammation: A landmark 2013 study by Borrelli et al. tested CBG in a mouse model of acute colitis (DNBS-induced colonic inflammation). They found CBG dramatically attenuated colitis severity – treated mice had less colon weight gain and ulceration, lower myeloperoxidase activity (an inflammation marker), and reduced expression of pro-inflammatory cytokines (IL-1β, IFN-γ) while increasing anti-inflammatory IL-10. CBG also normalized oxidative stress markers in the colon (elevating superoxide dismutase activity and reducing nitric oxide production). Mechanistically, some of these effects were linked to the endocannabinoid system: in macrophage cultures, CBG suppressed nitric oxide (NO) release and iNOS enzyme levels, an effect modulated by CB₂ receptors. (Blocking CB₁ had no effect, whereas blocking CB₂ unexpectedly enhanced CBG’s inhibition of NO, suggesting CBG might act as a partial agonist or inverse agonist at CB₂ in this context) Overall, CBG-treated colitic mice showed far less tissue damage and inflammatory biomarker elevation than untreated controls, leading the authors to conclude CBG “could be considered for clinical experimentation in IBD”. Indeed, this study provided a strong mechanistic rationale: CBG reduced inflammatory mediators and supported the gut’s antioxidant defenses and epithelial integrity in the face of inflammatory insult.
- Gut Barrier & Microbiome: Building on those results, recent research has examined CBG’s effects on the gut lining and microbial dysbiosis during intestinal inflammation. In 2024, Anderson et al. reported that an oral high-CBG hemp extract (containing ~20 mg/mL CBG, plus CBD and minor cannabinoids) markedly improved outcomes in a mouse model of IBD (dextran sulfate sodium colitis). Mice given daily CBG-rich extract during an active colitis episode had dramatically reduced disease severity: histological damage scores were lower, colon length (an index of inflammation-associated shortening) was longer, and clinical illness indices improved compared to controls. Notably, 16S rRNA sequencing of gut microbiota showed that CBG treatment shifted the microbiome toward a more normal composition after DSS-induced dysbiosis. Several inflammation-associated microbial changes were reversed – in essence, CBG helped rebalance the gut flora in a manner consistent with reduced colitis severity. Furthermore, metabolomic profiling of fecal samples indicated that CBG-treated mice had a normalization of key metabolic pathways related to inflammation (e.g. bile acid and eicosanoid metabolism), which are typically disrupted in colitis. Together, these findings suggest CBG not only dampens gut inflammation but also fortifies the intestinal barrier and promotes a healthier microbiome environment during disease. This dual action – immunomodulation and barrier support – is especially attractive for conditions like ulcerative colitis or Crohn’s disease, where both immune overactivation and loss of epithelial integrity drive pathology.
- Early Clinical Signal in IBS: While robust clinical trials in IBD are still forthcoming, a small proof-of-concept human study hints at GI benefits of CBG in tandem with CBD. In an open-label pilot trial in irritable bowel syndrome (IBS), six patients were given a twice-daily oral tincture containing 16.7 mg CBG + 16.7 mg CBD (total ~33 mg each per day) for 2 weeks. Five of six patients (83%) experienced a notable reduction in abdominal pain – mean pain scores fell by about one-third (from 6.6 to 3.7 on a 10-point scale) over the 14 days. Several patients also reported improved bowel habits (less pain upon defecation), though bloating symptoms persisted. Importantly, no adverse reactions were reported with this CBG/CBD regimen. While very preliminary (open-label and small N), this trial suggests combined phytocannabinoids could alleviate certain IBS symptoms, particularly visceral pain. It also reinforces the safety of CBG in the GI context, at least in the short term and in combination with CBD. These human observations align with the anti-inflammatory and analgesic effects seen in animal models, supporting further exploration of CBG or CBG-rich formulations in functional GI disorders.
Mechanistic considerations: CBG’s gut benefits seem to arise from a convergence of actions. Through CB₂ and other receptors in the colon immune cells, CBG can reduce production of nitric oxide and inflammatory cytokines. Through direct epithelial effects, it may tighten cell junctions and reduce oxidative injury to the mucosa. The fact that CBG also interacts with the gut microbiome (as seen by microbiota shifts in treated mice) is particularly intriguing – it raises the possibility that CBG fosters a microbiome that is less pro-inflammatory (for instance, increasing commensal bacteria that produce anti-inflammatory metabolites). All of these facets would be highly desirable in IBD therapy. Of course, controlled clinical trials are needed to confirm efficacy. Key questions – such as optimal dosing, the relative contribution of CBG vs CBD (in combo products), and long-term safety in the gut – remain unanswered. Still, the strong preclinical data provide a rationale to proceed. Plans are underway for randomized, placebo-controlled studies of CBG (and CBG/CBD) in conditions like ulcerative colitis and IBS, to formally test whether these promising effects translate to patients. If successful, CBG-based therapies could fill a gap by reducing gut inflammation and healing the mucosal barrier without the systemic immune suppression of current IBD drugs.
Antibacterial Activity: From Petri Dish to Potential Therapies
Perhaps the most surprising property of CBG is its antibacterial potency, particularly against difficult-to-treat pathogens. Cannabis has long been noted to contain antibacterial compounds, but recent studies have spotlighted CBG as an especially powerful antibacterial cannabinoid. Research teams in Canada and Europe have conducted detailed experiments showing CBG can kill drug-resistant bacteria, disrupt biofilms, and even work in vivo:
- Potent Anti-MRSA Effects: In 2020, Farha et al. reported that CBG exhibits strong activity against Staphylococcus aureus, including methicillin-resistant S. aureus (MRSA). In vitro, CBG had a low minimum inhibitory concentration (MIC) against MRSA and effectively prevented biofilm formation (biofilms are protective bacterial communities that resist antibiotics). Impressively, CBG could also eradicate pre-formed MRSA biofilms and kill “persister” cells – the dormant subpopulation of bacteria that often survives antibiotic treatment. Mechanistic assays revealed that CBG targets the bacterial cell membrane. It causes membrane disruption in Gram-positive bacteria, leading to leakage of cellular contents and rapid bacterial death. This membrane-lytic mechanism is analogous to how some polymyxin antibiotics work, and it is significant because it implies a low likelihood of bacteria developing easy resistance (destroying the membrane is hard for bacteria to bypass). The research went beyond the petri dish: in a mouse model of systemic MRSA infection, CBG treatment significantly reduced bacterial load, demonstrating in vivo efficacy as an antibiotic. A ScienceDaily summary of the work noted that CBG “proved to be marvelous at tackling pathogenic bacteria,” albeit with a caveat of some host cell toxicity at higher concentrations. Taken together, these findings established CBG as a lead compound in the search for new antibiotics.
- Broad-Spectrum and Synergy: CBG’s antibiotic action isn’t limited to staph. While Gram-negative bacteria are inherently more resistant (due to their outer membrane), CBG can still be effective when that barrier is circumvented. Farha et al. showed that if Gram-negative bacteria (like E. coli) are sensitized with a membrane-permeabilizer, CBG readily penetrates and kills them by disrupting the inner membrane. This suggests a role for CBG in combination therapies. In fact, CBG was found to synergize with polymyxin B (an antibiotic that punches holes in Gram-negative outer membranes): the combo potently killed multi-drug-resistant Pseudomonas and Acinetobacter strains in vitro. Beyond direct killing, CBG has been shown to inhibit quorum sensing and motility in certain bacteria, essentially “disarming” pathogens by preventing them from coordinating attacks or forming biofilms. For example, CBG disrupted quorum sensing signals in Vibrio harveyi at sub-inhibitory levels, curbing its biofilm formation without necessarily killing the bacteria outright. Such antivirulence effects could be valuable in preventing chronic infection scenarios. A 2025 review of cannabinoid antimicrobials highlighted CBG’s broad-spectrum potential and its ability to work in concert with conventional antibiotics. Unlike THC or CBD, which showed more modest or narrow antibacterial effects, CBG consistently stood out as one of the most potent cannabinoid antibacterials, especially against Gram-positive pathogensmdpi.com.
- Prospects and Challenges: The exciting antibacterial profile of CBG has prompted calls for new drug development efforts. CBG or CBG-derivatives could be explored as topical antimicrobials (for skin infections or wound dressings) or as coatings on medical devices prone to biofilm colonization (catheters, stents, etc.). These applications could leverage CBG’s strengths while minimizing systemic exposure. Indeed, one immediate idea is a topical CBG ointment for MRSA skin infections, which might eradicate bacteria in a wound without the need for systemic antibiotics. Another near-term possibility is using CBG as an adjuvant: combining it with existing antibiotics to break biofilms or to sensitize Gram-negative bacteria, as demonstrated with polymyxin B. However, translating CBG to a systemic antibiotic drug faces challenges. One issue highlighted by researchers is host cell toxicity – CBG’s membrane-disrupting action is not entirely selective for bacteria. At higher doses, it can damage mammalian cell membranes too, which was seen in cell culture and limits the achievable dose in vivo. The McMaster University team noted this “opens a therapeutic window, but a narrow one”. Medicinal chemistry will likely be needed to tweak CBG’s structure to retain antibacterial potency while reducing cytotoxicity. Additionally, extensive safety and ADME profiling of CBG must precede any clinical use as an antibiotic (to ensure it doesn’t, for example, cause hemolysis or organ toxicity at bactericidal doses). The good news is that so far MRSA has not been able to easily evolve resistance to CBG in laboratory studies, a promising sign, since many current antibiotics rapidly lose effectiveness to resistance. In summary, CBG represents a compelling new antimicrobial lead, with proven ability to kill drug-resistant bacteria and disrupt biofilms. Further research is ongoing to optimize its drug properties and assess its efficacy in animal infection models of skin, wound, or systemic disease. If these efforts succeed, CBG (or analogues) could one day join our antibiotic arsenal, addressing the urgent need for novel agents against resistant superbugs
Safety, Tolerability, and Limitations
While the therapeutic promise of CBG is evident, it is equally important to consider its safety profile, potential side effects, and gaps in current knowledge. As a relatively new compound on the clinical scene, CBG’s risk profile is not fully characterized, but several cautionary points can already be identified from preclinical studies and analogies to other cannabinoids:
- Cardiovascular Effects: CBG’s potent action on α2-adrenergic receptors means it can affect cardiovascular physiology similarly to other α2-agonists (which are known to cause vasodilation, bradycardia, and hypotension). Indeed, recent work by Arnold et al. demonstrated that CBG lowers blood pressure in mice via an α2-mediated mechanism. An acute dose of 10 mg/kg CBG significantly reduced mean arterial pressure in normal mice (though not as strongly as the pharmaceutical α2-agonist guanfacine), and this hypotensive effect was blocked by an α2-receptor antagonist, confirming the pathway. Chronic administration of CBG (10 mg/kg daily) likewise produced a sustained reduction in blood pressure in that study. These findings ring alarm bells for use in humans: CBG could cause lightheadedness, fainting, or dangerous drops in blood pressure, especially in susceptible individuals (elderly patients, those on antihypertensive medications, etc.). To date, the limited human data (e.g. the 20 mg acute study) did not report significant heart rate or BP changes, but these trials have been small and in healthy subjects. As larger trials progress, vital sign monitoring will be crucial. It may be that CBG’s cardiovascular effects are mild at low doses but become pronounced at higher exposures. Until more is known, clinicians should approach CBG cautiously in patients with cardiovascular vulnerabilities, and future studies are prioritizing cardiovascular safety monitoring (measuring heart rate, BP, EKG changes, etc.).
- Drug–Drug Interactions: Many cannabinoids are known to interact with drug metabolism enzymes, and CBG is no exception. In particular, cannabinoids can inhibit cytochrome P450 isozymes like CYP2C9 and CYP2C19, which are responsible for metabolizing a variety of medications (e.g. the anticoagulant warfarin, many anticonvulsants, and sedatives). There is concern that CBG supplements could alter the blood levels of co-administered drugs by inhibiting their breakdown. While specific data on CBG’s P450 inhibition potency are still being gathered, its structural similarity to CBD (which strongly inhibits CYP2C19 and CYP2C9) suggests caution. A published case report on cannabinoid use and warfarin, for example, found significantly elevated INR (bleeding risk) when patients also used cannabinoids that likely inhibited warfarin’s metabolism. We should assume CBG could have similar interactions, pending confirmation. Additionally, CBG’s effect on CYP3A4 and other enzymes is not yet clear – if it inhibits CYP3A4, it could interfere with the metabolism of a large number of drugs (statins, calcium channel blockers, etc.). Until definitive studies are done, patients on critical medications should either avoid CBG or use it only under medical supervision, with potential drug level monitoring. On the flip side, CBG itself is metabolized by P450 enzymes (recent in vitro work showed human liver microsomes rapidly oxidize CBG into several metabolites). Thus, inducers or inhibitors of P450s might alter CBG’s own levels. All these interactions need systematic study. This is an area of active research, and early Phase I pharmacokinetic trials are measuring not only CBG’s half-life and clearance but also any changes in activity of CYP enzymes when CBG is present.
- High-Dose and Chronic Exposure Risks: As with many drugs, dose makes the poison for CBG. While low- to moderate-doses have shown good tolerability, very high doses might reveal toxicity. In one notable mouse study (Aljobaily et al., 2022) examining CBG in a non-alcoholic steatohepatitis (NASH) model, a low dose of CBG (2.5 mg/kg/day) was beneficial – reducing liver inflammation and fibrosis – but a high dose (25 mg/kg/day) actually worsened liver outcomes. Mice receiving the high CBG dose had increased hepatic inflammation, more fibrotic scarring, and greater liver cell damage compared to controls. This kind of U-shaped dose response is a red flag, suggesting that beyond a certain threshold, CBG might overload physiological systems or engage off-target effects that cause harm (for instance, excessive α2-mediated reduction of blood flow to organs, or buildup of toxic metabolites). It underscores the importance of defining a therapeutic window for CBG – the range between an effective dose and a toxic dose. Importantly, the doses used in mice don’t directly translate to humans, but this study provides a proof that “more is not always better” with CBG. Long-term high-dose CBG exposure could potentially stress the liver (as indicated by elevated ALT/AST enzymes in some reports) or other organs. Therefore, escalating doses in clinical trials must be done carefully, with frequent lab tests (liver and kidney function, etc.). Regulatory guidance for CBD (a similarly classed supplement) already warns of liver enzyme elevations at high doses; CBG may show a similar pattern. Additionally, chronic use needs study – e.g. will daily CBG for months affect hormone levels, immune function, or reproductive parameters? These are open questions. As of now, no chronic toxicity in animals or humans has been published beyond a few weeks, so significant data gaps remain regarding long-term safety.
- Other Side Effects and Special Populations: Thus far, reported side effects of CBG (short-term use) are mild – some users have noted dry mouth or increased appetite, and preclinical studies indicate possible sedation at higher doses (expected from α2-agonism). Unlike THC, CBG is non-intoxicating, so we don’t worry about psychoactive adverse effects or addiction potential in the same way. However, subtle neuropsychiatric effects (mood alterations, sedation, etc.) should be monitored. Sedation could especially be an issue if CBG is combined with other CNS depressants. Another aspect to consider is pediatric or perinatal use – these have not been studied at all, and developing nervous systems might react differently to a compound that modulates neurotransmitter receptors. Thus, CBG should be avoided in children or pregnant women until more is known. Similarly, immunocompromised patients or those with severe illnesses were not represented in any CBG studies; while CBG has anti-inflammatory properties, we need to ensure it doesn’t over suppress immune function or interact adversely with other treatments in such populations.
Finally, regulatory quality and purity are a concern. CBG is already sold as an unregulated supplement in some markets, meaning some products could contain contaminants or incorrect doses. Researchers stress that if CBG is to become a real medicine, robust manufacturing controls and pharmaceutical-grade formulation will be required. This includes formulating CBG for optimal bioavailability (since cannabinoids are lipophilic and can have variable absorption). For instance, a recent human pharmacokinetic study found that taking CBG with a high-fat meal dramatically increased its plasma levels relative to fasting. Formulations like lipid-based emulsions or nanoparticle carriers might achieve more consistent absorption and exposure. Such innovations will be important for standardizing dosing in clinical use.
Future Directions and Conclusion
CBG is emerging as a multifaceted therapeutic candidate – not just another minor cannabinoid, but one with a distinct spectrum of actions spanning the nervous system, immune system, and even direct antimicrobial effects. The evidence to date (though early) marks CBG as a credible lead for a variety of conditions: anxiety and stress-related disorders, inflammatory bowel disease, antibiotic-resistant infections, and possibly neurodegenerative or metabolic diseases. Its unique receptor binding profile (weak at CB₁/CB₂, strong at α2/5-HT1A) offers a mechanism to achieve effects that cannabinoids like CBD or THC alone may not produce – e.g. reducing anxiety while enhancing alertness, or fighting bacteria via membrane disruption.
That said, we must emphasize caution and rigor moving forward. The current data, while highly encouraging, come largely from preclinical models and very limited human trials. We have yet to see large-scale, placebo-controlled clinical trials that prove CBG’s efficacy for any indication. These are now on the horizon: teams are planning Phase II studies in generalized anxiety disorder (dosing CBG in the 20–50 mg range over several weeks) and in inflammatory conditions like ulcerative colitis (possibly using CBG-enriched formulations as adjunct therapy). There is also interest in topical or localized uses, such as CBG-based creams for dermatological inflammation or infection. Alongside efficacy trials, dedicated pharmacokinetic (PK) and pharmacodynamics (PD) studies are needed. Key questions include: What is CBG’s oral bioavailability and half-life in humans? (Animal data suggest a half-life of a few hours, but human metabolism can differ.) Through which pathways is it metabolized and cleared? Does it induce or inhibit any enzymes over time? Answering these will inform safe dosing regimens and identify any drug interaction risks early.
Another active area will be formulation science – improving how CBG is delivered. Researchers are exploring lipid encapsulation, cyclodextrin complexes, and even prodrug approaches to enhance CBG’s solubility and tissue targeting. For instance, a liposomal CBG might yield higher tissue concentrations in the gut (for IBD) or better skin penetration (for an antibacterial gel). Combination therapies are also on the table: given CBG’s synergy with polymyxin for Gram-negative bugs, or its potential synergy with CBD or terpenes for pain/inflammation, future products might intentionally blend compounds to maximize benefit (as was done in the small IBS trial). Of course, any combinations will require careful testing to ensure additive benefits without additive toxicity.
Safety monitoring will remain front-and-center as CBG moves through trials. Particular focus will be on cardiovascular parameters (blood pressure, heart rate) due to the α2 effect, and on hepatic enzymes (to catch any liver stress early). Regulatory agencies will likely require chronic toxicity studies in at least two species before green-lighting long-term human use. Given the hints of dose-dependent liver effects in mice, human studies will probably start at conservative doses and only escalate slowly with oversight. It will also be important to study special populations (eventually): Are the elderly more sensitive to CBG’s effects? Does CBG pass into the brain readily (and could it accumulate)? Does it affect fertility or development? These questions remain unanswered for now.
In conclusion, CBG stands at an exciting intersection of modern pharmacology and cannabinoid science. It has shown therapeutic promise across multiple domains – from calming the anxious mind and protecting neurons, to damping gut inflammation and killing superbugs. Such a wide-ranging profile is rare and merits thorough exploration. Yet we must balance enthusiasm with scientific rigor: robust clinical evidence is needed to substantiate each claimed benefit, and safety must be demonstrated with the same rigor as efficacy. The next few years should see an expansion of CBG research, including larger human trials and deeper mechanistic studies. If outcomes are positive, CBG could progress from an experimental compound to a prescription-grade API (active pharmaceutical ingredient) for specific indications. Conversely, if any red flags emerge (inefficacy or toxicity), that will inform us of CBG’s limitations. Either way, the ongoing studies will greatly enrich our understanding. As one review aptly noted, unlike CBD, little research has been done on this unregulated molecule, and much of what is “known” still warrants confirmation – further investigation will identify both its potential therapeutic uses and any hazards. In effect, we are now doing the careful work to turn early promise into proven science. The bottom line: CBG is a novel and compelling candidate in several fields of medicine, but it is not yet a proven therapy. With rigorous clinical research and meticulous development of safe formulations, we will learn exactly where CBG can be beneficial and how to harness it responsibly. The story of CBG is just beginning, and as fellow researchers and clinicians, we should critically examine the data as it emerges – challenging claims, reproducing results, and ultimately building the evidence base together for this intriguing minor cannabinoid.
Sources:
-
Cascio et al. Brit. J. Pharmacol. (2010) – “Evidence that cannabigerol is a highly potent α<sub>2</sub>-adrenoceptor agonist and moderately potent 5-HT<sub>1A</sub> receptor antagonist.” Key results on CBG’s receptor binding profilepmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov.
-
Cuttler et al. Sci. Reports (2024) – “Acute effects of cannabigerol (CBG) on anxiety, stress, and mood: a double-blind, placebo-controlled, crossover trial.” First human trial showing reduced anxiety/stress and improved memory with 20 mg CBG, no impairmentpmc.ncbi.nlm.nih.govnews-medical.net.
-
Borrelli et al. Biochem. Pharmacol. (2013) – “Beneficial effect of cannabigerol on experimental inflammatory bowel disease.” CBG reduced inflammation and oxidative stress in murine colitis; suggests CB₂-related mechanismspubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov.
-
Anderson et al. J. Pharmacol. Exp. Ther. (2024) – “High-CBG hemp extract moderates colitis and modulates the microbiome in an IBD model.” CBG-rich extract lowered colitis severity in DSS mice and normalized gut microbiota and metabolitespmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov.
-
Good et al. Am. J. Gastroenterology (2023) – Abstract S648: “Open-label trial of CBD/CBG in IBS.” Six-patient pilot showing ~33% pain reduction in IBS with CBG/CBD therapy, with no adverse eventsjournals.lww.comjournals.lww.com.
-
Farha et al. ACS Infect. Dis. (2020) – “Uncovering the hidden antibiotic potential of cannabis.” Demonstrated CBG’s potent activity against MRSA: inhibits biofilms, lyses cells by membrane disruption, effective in MRSA-infected micepubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov.
-
ScienceDaily (McMaster Univ.) – “Researchers uncover hidden antibiotic potential of cannabis” (Feb 26, 2020). Summary of Farha et al. findings: CBG kills MRSA biofilms and persisters by targeting bacterial membranessciencedaily.comsciencedaily.com.
-
Li et al. Molecules (2024) – “Cannabigerol: A comprehensive review of molecular mechanisms and therapeutic potential.” Recent review covering CBG’s effects on inflammation, antibacterial action, and cardiovascular findings in micemdpi.commdpi.com.
-
Nachnani et al. J. Pharmacol. Exp. Ther. (2021) – “The Pharmacological Case for Cannabigerol.” Review article noting CBG’s unique receptor targets and potential in neurologic disorders and IBD, while calling for more research into its safety and efficacypubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov.
-
Wikipedia – “Cannabigerol” (accessed 2025). Summarizes CBG’s pharmacodynamics (partial CB₁/CB₂ agonist, α<sub>2</sub>-adrenergic agonist, 5-HT<sub>1A</sub> antagonist) and mentions safety concerns about sedation and blood pressureen.wikipedia.orgen.wikipedia.org.


